Did you know that in the United States, around 65.3% of women aged 15 to 49 use contraception?¹ Birth control helps with preventing unplanned pregnancies, as well as regulating menstrual cycles, and alleviating problems like heavy bleeding and severe cramps.
Millions of women around the world are facing the challenges of uterine fibroids, and many wonder how birth control might impact their condition. Whether you’ve already been diagnosed or are at higher risk, it’s important to understand the potential benefits and drawbacks. Let’s explore how birth control can help manage fibroid symptoms and address your concerns.
If you are experiencing painful periods that limit your daily activities, it might be time to talk to a fibroid specialist.
Our fibroid specialists at USA Fibroid Centers can answer your questions about fibroids and birth control while evaluating your health to make a personal treatment plan.
CONSULT WITH A FIBROID SPECIALIST
Did you know abnormal bleeding (anything that deviates from your regular pattern) is one of the most common symptoms of fibroids? If you are bleeding between periods, have heavier or longer menstrual bleeding than usual, or experience severe pelvic pain, uterine fibroids may be the cause.
Other fibroid symptoms include:
- An enlarged uterus
- Pelvic or lower back pain
- Anemia-induced fatigue
- Painful sexual intercourse
- Frequent urination
- Severe cramps
Fibroids are a type of noncancerous tumor that commonly develops in or on the uterus. Up to 70% of U.S. women develop uterine fibroids during their lifetime, with women experiencing symptoms ranging from mild to severe.²
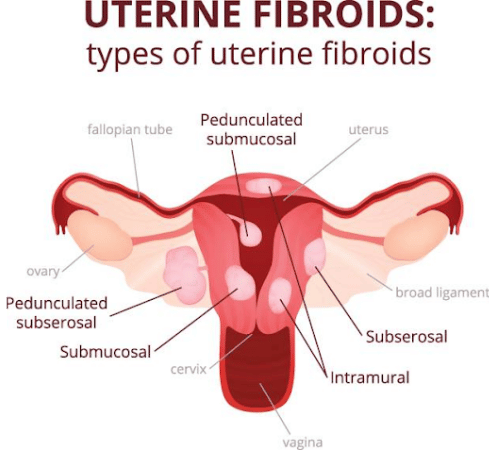
There are five fibroid types:
- Intramural Fibroids: grows in the muscular walls of the uterus
- Subserosal Fibroids: develop outside the uterus
- Submucosal Fibroids: occur within the uterus’s inner lining
- Pedunculated Fibroids: attach to the uterine wall by a peduncle or stalk and can develop inside or outside the uterus.
- Calcified Fibroids: form after a fibroid outgrows its blood supply and experiences fibroid degeneration.
The definite cause of fibroids is unknown, although research indicates that genetic, hormonal, and other factors may play a role. Due to the widespread use of hormonal birth control and the commonality of fibroids, it is understandable to wonder about the relationship between fibroid growth and birth control.
How Birth Control Methods Impact Fibroids
While fibroid growth is not completely understood, research has demonstrated a link between fibroids and hormones. If you already have fibroids, taking birth control pills (especially high-strength ones) may help alleviate symptoms like heavy periods and severe cramps but may also lead to additional fibroid growth.
Hormonal birth control, such as pills, patches, injections, and IUDs, can have varying effects on fibroids. While it may not directly shrink fibroids, hormonal birth control can help manage symptoms in some women. Consulting with a doctor is crucial to determine the most suitable birth control option based on your overall health and specific risk factors.
Birth Control Pills
One of the most popular forms of contraceptive is the hormonal birth control pill, which comes in two main types. The first is a full-strength pill that combines estrogen and progestin (synthetic progesterone), and the second only uses progestin. The progestin-only type is commonly known as the “mini-pill.”
Both types of birth control pills work by preventing fertilization, which occurs when an egg and sperm join together. In the case of the full-strength pill, the hormones aim to keep the body from ovulating (releasing an egg) in the first place.
With the mini pill, the hormones it releases thicken the mucus in and around the cervix, which stops sperm from passing through it successfully.
Lastly, some birth control pills can change the lining of the womb so that a fertilized egg will most likely not be implanted.
Even though many doctors prescribe the pill as a form of birth control that reduces fibroid symptoms, they do not minimize or remove fibroids. It’s important to discuss with your doctor the risk of fibroids and birth control pills.
Intrauterine Devices (IUDs)
Another popular form of birth control for fibroids is IUDs. An intrauterine device (IUD) is a small, T-shaped device inserted into the uterus to prevent pregnancy. It is highly effective and considered a long-acting reversible contraceptive (LARC). There are two main types of IUDs:

Hormonal IUDs (e.g., Mirena, Kyleena): These IUDs release progestin, which thins the uterine lining, thickens cervical mucus, and partially suppresses ovulation. This can often reduce heavy menstrual bleeding and cramping.
Non-hormonal IUDs (e.g., Paragard): This type of IUD releases copper to create a toxic environment for sperm, which may increase bleeding and cramping and create issues for those with fibroids.
Women with fibroids can generally use IUDs, and hormonal IUDs may help reduce symptoms like heavy bleeding. However, IUDs do not cure fibroids or prevent their growth. There is also a higher risk of IUD expulsion in women with fibroids.³
While an IUD can provide symptom relief, it is not a treatment for fibroids, and symptoms may return once the IUD is removed. That is why talking to your doctor about the different kinds of contraceptives and their impact on your hormones is especially important if you have fibroids.
Injections and Implants
When it comes to fibroids and birth control, other options are injections and implants. Injections and implants are types of Long-Acting Reversible Contraception (LARC)that differ in duration and side effects. Injection and implant contraceptives include:
- Depo-Provera (Injection): A progestin injection administered every three months. It can cause irregular bleeding, menstrual changes, and fertility delays for up to a year. It may shrink fibroids but could also cause them to grow.
- Nexplanon (Implant): A small rod is inserted under the skin of the upper arm, effective for up to five years. It may cause a range of side effects, including irregular bleeding, weight gain, and mood changes. It is less likely to increase fibroid growth than hormonal birth control pills.
While hormonal birth control can be a helpful option for managing fibroid symptoms, the choice depends on individual circumstances or your individual situation. Some women with fibroids may not be able to use hormonal birth control due to underlying health conditions such as a history of breast cancer or severe liver disease.
Barrier Methods

Barrier methods are a form of birth control that physically prevents sperm from reaching the egg and include condoms, diaphragms, cervical caps, sponges, and vaginal spermicides. They do not affect hormone levels.
These birth control methods are generally safe and effective while also available for purchase without a prescription. They do not affect fibroids, which also means they will not help reduce fibroid symptoms.
What’s The Best Birth Control for Fibroids?
Taking either a full-strength pill (estrogen and progestin) or a mini pill (progestin only) can help reduce menstrual bleeding whether or not you have uterine fibroids.
Low-dose birth control pills contain fewer hormones than regular pills and are not believed to cause fibroid growth. They are effective at preventing pregnancy and tend to have fewer side effects and risks than higher-strength birth control pills.
If you’re trying to avoid fibroid growth, the best birth control with fibroids may be a low-dose pill. However, regular strength birth control pills may offer better control of your fibroid symptoms and slightly more effective protection against pregnancy.
Along with discussing the use of birth control for fibroids with a medical provider, we recommend exploring fibroid treatment options with a fibroid specialist. Our experts at USA Fibroid Centers can inform you of your available treatments.
What Happens to Fibroids When Birth Control is Stopped?
While hormonal birth control can help manage fibroid symptoms in some cases, it doesn’t directly treat the fibroids themselves. Therefore, stopping birth control can sometimes lead to:
- Return of symptoms: Fibroid symptoms, such as heavy bleeding, pelvic pain, and pressure, may return or worsen after stopping birth control.
- Fibroid growth: In some cases, stopping birth control can lead to the growth of new fibroids or the enlargement of existing ones.
- Increased risk of pregnancy: If a woman with fibroids stops taking birth control without planning to get pregnant, she may be at increased risk of an unplanned pregnancy, which can further complicate her condition.
It’s important for women with fibroids to discuss these concerns with their healthcare provider before making any decisions about stopping birth control. They can help assess the individual risks and benefits of continuing or discontinuing birth control and recommend appropriate treatment options.
Fibroids and Birth Control: Finding the Right Treatment

If you are taking birth control for fibroids and your symptoms aren’t improving or are worsening, you may be looking for alternative solutions. While surgical treatments may be recommended, these are not your only options.
Uterine Fibroid Embolization (UFE) is a safe, effective alternative to surgery that allows women to shrink their fibroids without having their uterus removed.
UFE has been shown to significantly reduce fibroid size, leading to improvements in heavy bleeding, pelvic pain, and pressure. Unlike surgery, UFE doesn’t require anesthesia or hospitalization, making it a convenient and less invasive option.
SCHEDULE BY CALLING 855.615.2555
What to Expect at A Fibroid Consultation
If you have questions about birth control and uterine fibroids, our fibroid specialists can help. USA Fibroid Centers provides UFE treatment nationwide to help you get long-lasting relief.
A fibroid consultation is an appointment with a healthcare professional who specializes in treating uterine fibroids. During this appointment, you’ll discuss your symptoms, medical history, and potential treatment options.
No matter where you book your appointment, we look forward to helping you improve the quality of your life. To learn more, call 855.615.2555 or schedule an appointment online.
Sources
- Data Briefs, National Center for Health Statistics, Centers for Disease Control and Prevention
- “Epidemiology and management of uterine fibroids,” International Journal of Obstetrics and Gynecology
- “Intrauterine device use among women with uterine fibroids: A systematic review,” Contraception